Aortic aneurysms
What is an Abdominal Aortic Aneurysm (AAA)?
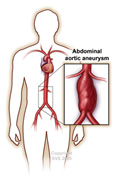
The aorta is the largest artery in your body. It is a muscular vessel that transmits oxygen-rich blood from the heart to the lower abdomen. In the chest, it is called the “thoracic aorta”. In the abdomen, it is referred to as the “abdominal aorta”. At the level of your belly button (umbilicus), the aorta divides into two iliac arteries that carry blood through the pelvis and into each leg.
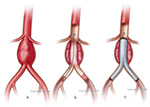
When the wall of a blood vessel weakens, internal pressure causes it to expand or bulge like a balloon. This abnormal dilatation is called an “aneurysm”. When this occurs in the abdominal aorta, the result is an Abdominal Aortic Aneurysm or AAA. 75% of aortic aneurysms are found in this position. As might happen with a balloon, an increase in aneurysm diameter can result in it bursting (rupture). Aneurysm rupture is a surgical emergency. It generally results in severe internal bleeding, causes collapse from shock and carries a high risk of death. Life-saving surgery is then required.
Clearly, there is a benefit to having an AAA treated well before it bursts, provided that your surgeon is able to offer its repair with acceptably low complication rates. The published mortality rate for elective AAA repair in Australia is < 4%. A/Professor McClure’s experience of treating over 375 AAA by either open surgery or endografting over the past 14 years, has been accompanied by a 30-day operative mortality of 0.8%. It is essential that the Vascular Surgeon you see for repair of your AAA provides you with their own outcome figure for you to consider.
|
|
| Abdominal Aortic Aneurysm |
How do I know if I have an aneurysm (the symptoms)?
For most people, a growing AAA causes no symptoms. The vast majority is found by chance during a test for an unrelated medical problem, and this leads to a referral for management by a Vascular & Endovascular Surgeon.
On occasions patients may be aware of the following:
- Pulsation in the upper abdomen, much like a heartbeat.
- Fullness or discomfort after eating.
- Pain, or ulceration, in the legs from material that breaks from the aneurysm and travels downstream to block arteries in the legs (embolisation).
- Severe and sudden pain in the abdomen, lower back or pelvis. This may be a sign of imminent rupture and is an indication for seeking URGENT medical attention.
What is the cause of an Abdominal Aortic Aneurysm?
While there continues to be active research into this matter, the exact cause of aortic aneurysmal degeneration remains unknown. Clearly, there is a genetic basis, and enzyme defects in the aneurysm wall that permits the breakdown of its components have been found. In the majority of patients, AAAs are also associated with generalised atherosclerosis (hardening of the arteries) throughout the body. While we have yet to identify measures to prevent aneurysms, reducing risk factors contributing to atherosclerosis, such as high blood pressure (hypertension) and smoking, is essential.
Recognised risk factors for AAA include:
- Gender: 80% of AAAs are found in men.
- Advancing age: AAAs are uncommon below the age of 60 years.
- Family history: Having a close relative with an AAA increases your risk of AAA and is a reason to have your own aortic diameter checked.
- Hypertension: Having high blood pressure puts increased strain on your aortic wall.
- Cigarette smoking: There is strong evidence that this increases the aneurysm growth rate. When you see A/Prof McClure regarding your AAA, he will advise that you stop smoking if this is a habit of yours.
Diagnosis: What tests are needed?
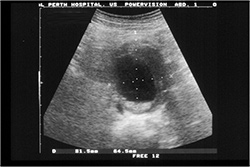
As mentioned, an AAA is usually found incidentally by routine physical examination or by a test such as ultrasound, CT scan, MRI, or plain abdominal x-ray. If your GP is concerned about the test finding, you may be asked to see a Vascular & Endovascular Surgeon. Further tests may then be needed to determine if surgery is required, if you are fit to undertake this surgery, and which of the surgical options are best for you.
 |
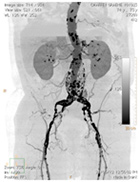 |
| An ultrasound image of AAA | CT scan result of an AAA |
What are the treatment options for an Abdominal Aortic Aneurysm?
Ongoing surveillance
An aneurysm will not disappear by itself, but its rate of growth varies. Between a diameter of 4.0 cm and 5.0 cm, the average growth rate is 1.0 cm per year. Above an AAA sac diameter of 5.0 cm, elective repair is usually considered. When an AAA has a diameter below this threshold, regular surveillance is recommended. This will be offered to you at Geelong Vascular Ultrasound on our ultrasound surveillance program. If you choose to be involved in this program, A/Prof McClure can keep an eye on the progress of your AAA, and recommend surgical treatment when it becomes necessary. It is crucial to continue follow ups as directed because the aneurysm may enlarge to a dangerous size over time and burst inadvertently.
Surgical treatment
Before surgery
Prior to planned surgery with A/Prof McClure, a number of tests will be undertaken, changes to your medication recommended, and admission details discussed with you. Please be sure that you understand the nature of the surgery to be undertaken and its associated risks before committing to your procedure. An anaesthetist, who will explain the type of anaesthetic to be used and its particular risks, usually supports surgery.
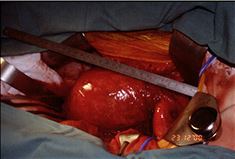
Open surgical aneurysm repair
Before the early 1990s, open surgical repair was the only option for fixing an AAA. This operation has to be performed under general anaesthetic and requires a long incision in the abdomen to provide access to the aneurysm. The weakened aortic wall is replaced with a prosthetic graft, which the body accepts well and through which blood flows freely. It replaces the diseased aortic segment. All patients need support in an Intensive Care Unit postoperatively for a few days, begin eating normally when bowel function returns in 4-5 days, and leave hospital after 10-14 days. This is major surgery and patients often take an extended period (6 weeks to 3 months) to return to normal activity. Postoperative instructions will be provided to you at the time of your operation.
 |
 |
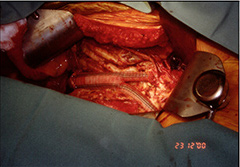 |
| AAA Sac | Inlay grafting of AAA |
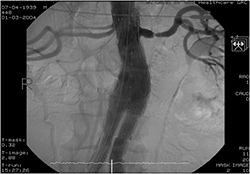
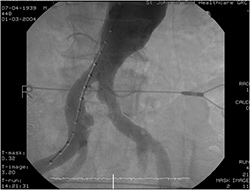
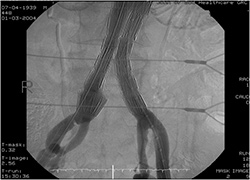
Endovascular stent grafting
Consistent with the move across many surgical fields for minimally invasive intervention, there is now a modern approach to AAA exclusion by use of endoluminal stent grafting. The principle of an “endovascular” approach is that treatment is undertaken inside arteries, by means of wires and catheters that are negotiated through the blood vessels. The procedure for AAA exclusion is undertaken through a small incision in each groin. Under X-ray control, an endograft (comprising the same material as used for open surgery but reinforced with self-expanding metal stents) is passed to the site of the aneurysm. It is positioned to achieve a seal above and below the aneurysm sac, thereby stopping flow into the dilated artery segment. Artery flow passes only through the graft, and this serves to reinforce the vessel wall so that it does not burst. While not all surgeons are trained in this technology, all dedicated Vascular Surgical Units across Australia now offer endografting to patients with AAAs that have suitable anatomy. In recent years, A/Prof McClure has found that 85% of his patients can be treated this way. In the others, open repair proves to be necessary.
 |
 |
| Endoluminal stent graft | Endoluminal stent grafting |
Endoluminal stent grafting of AAA can be performed under regional anaesthetic. Few patients require Intensive Care Unit support. All patients are able to eat on the first postoperative night, and most patients are discharged on the second or third postoperative day. As the operation is undertaken through small incisions in each groin, the return to normal activity is much quicker than following open repair.
 |
 |
 |
 |
The decision on the treatment approach most suitable for your AAA will be one A/Prof McClure helps you make. Each carries specific risks which will be discussed with you preoperatively and which are listed in the brochure you receive as a guide for patients on Surgical Treatment of an Abdominal Aortic Aneurysm. Please read the list of possible complications carefully and discuss any you do not understand with A/Prof McClure before your operation. At Geelong Vascular Service, it is our practice to follow the success of your treatment with regular surveillance ultrasound studies. This program will be organised for you at the time of your first postoperative visit and expresses the partnership we share with you in managing your vascular disease.