Carotid artery disease and stroke
What is carotid artery disease?
The carotid arteries are the main blood vessels in the neck responsible for carrying oxygenated blood from the heart to the brain. The lining of these arteries is normally smooth, permitting unobstructed flow through them. With age, plaque (composed of cholesterol, calcium, fatty cells and fibrous tissue) can become deposited in the vessel wall, much as rust might build up in a pipe. This plaque build-up causes the carotid arteries to become diseased by making them harder and narrow, which can lead to stroke or death. The risk of this consequence is determined by the degree of narrowing in the artery and by whether there have been “warning signs” of an impending neurological event.
 |
| Removed carotid artery plaque |
Plaque in an artery is prone to cracking under the stress of blood flow, and the body responds to this by forming a clot on the disrupted plaque surface. This clot may be so extensive that it blocks the artery. Alternatively, it may become dislodged, with or without a piece of the plaque, and travel downstream to a smaller artery within the brain substance. If it blocks this artery, oxygen supply beyond it stops. The brain cells in that territory stop working. If the body successfully breaks up the blockage and restores forward flow through the artery, the neurological disturbance is temporary. This is called a Transient Ischaemic Attack (or TIA) if the problem lasts less than 24 hours. If the body is unable to restore flow quickly, and the deficit lasts more than 24 hours, a permanent Stroke (or CVA) is said to have occurred.
What are the warning signs (symptoms)?
In many people, a high-grade narrowing in a carotid artery causes no symptoms until a major stroke or death occurs. These patients are regarded as being asymptomatic and are identified by a physician hearing a noise in the neck from the turbulence of flow through the narrowed artery or by an ultrasound test undertaken for generalized disease assessment. Other patients are symptomatic from a clinical warning sign. These include:
- Weakness or numbness of the face, arm or leg on one or both sides of the body
- Difficulty speaking or understanding directions
- Dizziness, loss of balance or an unexplained fall
- Loss of vision, sudden blurring or decreased vision in one or both eyes
- Headache, usually severe and abrupt in onset or an unexplained change in the pattern of headaches
- Difficulty swallowing
Any one of these symptoms may be a sign of an impending stroke and should be a prompt for seeking urgent medical attention. Call 000.
Diagnosis: What tests are needed?
Duplex carotid ultrasound: If your attending physician has concerns about your carotid arteries, the first test undertaken is an neck ultrasound. This can be performed at Geelong Vascular Ultrasound and is noninvasive and painless. It simply involves having an ultrasound probe applied to the neck so that flow through the carotid arteries and the nature of plaque, if present, can be imaged. In most cases, the result of this test provides all the information required for a decision to be made on the need for surgical treatment.
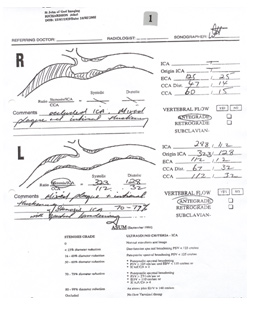 |
 |
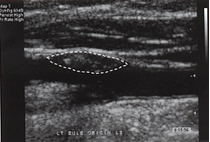 |
| Geelong Vascular Ultrasound | Image of carotid plaque |
Planning tests: If surgery to the carotid arteries is indicated, further imaging may be necessary to plan for the treatment. This will be organized by A/Prof McClure and may comprise:-
- CT angiography
- Magnetic resonance angiography (MRA)
- Digital subtraction angiography
A/Prof McClure will explain the need for these tests, their nature and risks when he orders them for you.
How is carotid artery disease treated?
Risk factor reduction
To reduce the progression of carotid artery disease, the following measures are often recommended:
- Reduce alcohol intake
- Exercise regularly to reduce weight
- Stop smoking
- Monitor your blood pressure, blood sugar and cholesterol levels regularly
- Follow your doctor’s treatment for high blood pressure, diabetes and heart disease
- Eat healthy food and avoid eating fatty food stuffs
Treatment options
Medical therapy:
Medicines that prevent platelet aggregation and the formation of clots are usually prescribed for patients at risk of stroke. These include aspirin and clopidogrel.
Surgery:
Surgery to treat carotid artery plaque is usually offered if the narrowing in the affected artery is more than 70% and the patient is asymptomatic, or greater than 50%, with symptoms of TIA or stroke. Treatment may be affected by removing the plaque by open surgery on the artery, a procedure called carotid endarterectomy. Alternatively, carotid angioplasty and stenting can stabilise the plaque and improve luminal calibre. The choice of treatment will be dictated by the nature of the disease, the shape of the carotid arteries, and the patient’s overall condition.
- Carotid endarterectomy: Open surgical removal of the diseased plaque is undertaken in the operating room. A/Prof McClure usually performs it under local anaesthetic, as this provides the best way of monitoring neurological function during the procedure. On rare occasions, treatment under general anaesthetic may be required. An incision is made on the side of the neck, and the affected arteries are exposed. These arteries are clamped, adequate arterial supply to the brain is ensured, the disease is removed, and the artery is closed, often with a prosthetic patch. The neck wound is closed with dissolving sutures. The operation usually takes 60 – 90 minutes, and most patients are able to leave hospital on the second postoperative day.
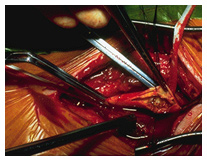 |
 |
| Carotid endarterectomy | Carotid angioplasty & stenting |
- Carotid angioplasty and stenting: In selected patients considered at high risk for carotid endarterectomy, stenting of the carotid artery disease may be offered. In A/Prof McClure’s practice, this is confined to those who have recurrent stenosis, have a hostile neck from previous surgery or radiotherapy, or are too medically fragile to be able to tolerate open surgery under local anaesthetic. This approach involves a groin puncture under local anaesthetic, and passage of catheters into the neck. Disease in the affected carotid artery is traversed with a tiny filter to protect the brain from plaque debris and then treated with a suitably sized stent. This procedure takes place in an angiography suite, and usually takes 20 – 30 minutes. Most patients are able to leave hospital on the following day.
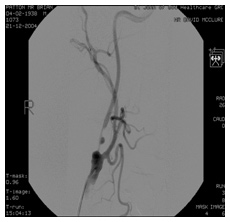 |
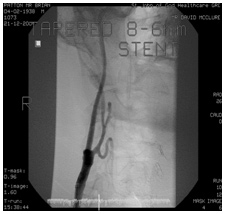 |
| Narrowed carotid artery | Treated artery after stenting |
Should you need treatment for your carotid arteries, you should ensure that your surgeon is able to offer it with acceptably low complication rates. The Australian published stroke and death rate following carotid endarterectomy is 1.7%. A/Professor McClure’s experience of treating over 785 cases by either open endarterectomy or stenting over the past 14 years has been accompanied by a combined stroke and death rate of 0.9%. It is important that the Vascular Surgeon you see for treatment of your carotid artery disease is able to provide you with their own outcome figure for you to consider.
The decision on the treatment approach most suitable for your carotid artery disease will be one A/Prof McClure helps you make. Each carries specific risks which will be discussed with you preoperatively and which are listed in the brochure you receive as a guide for patients on Carotid Endarterectomy and Angioplasty with Stenting. Please read the list of possible complications carefully and discuss any you do not understand with A/Prof McClure before your operation. At Geelong Vascular Service, it is our practice to follow the success of your treatment with regular surveillance ultrasound studies. This program will be organised for you at the time of your first postoperative visit and expresses the partnership we share with you in managing your vascular disease.
