Leg ulcers
Management of lower limb ulceration
At Geelong Vascular Service, we often see patients with recalcitrant leg ulcers who have failed to improve despite various dressings. It may be instructive to consider how we might be able to assist patients at an earlier stage of their healing process.
 |
 |
Aetiology
All leg “ulcers” (this term is used for any loss in an epithelial surface) are caused by trauma. The trauma may be overt or innocuous, acute or chronic, iatrogenic or the result of unrelieved pressure. Over an ulcer, in healthy tissue, complete epithelial cover should take place within 4 weeks; the surface dressing choice is dictated by whether the wound is wet or dry. If an ulcer persists beyond this time frame, underlying pathology must exist, which inhibits epithelial cell growth. In 85% of leg ulcers, prolonged healing is the consequence of arterial or venous disease; the former is responsible for impaired oxygen delivery to the skin, and the latter for limb oedema or scarring that limits oxygen diffusion to the ulcer base. It follows that, in these patients, early vascular assessment is critical to limit tissue loss and to identify treatment options. In only a small percentage of patients is infection, malignancy, or neuropathy the primary problem.
The Vascular Ulcer
Leg ulcers are often described as being “arterial”, “venous”, or “mixed” if the reason for their persistence is arterial compromise, venous incompetence or obstruction, or a mixture of both, respectively. With the availability of minimally invasive techniques to manage vascular disease, usually under local anaesthetic, very few patients now cannot be offered some therapy to improve the health of their legs and the capacity to heal their ulcers. Patients are never “too old” for treatment!
Treatment strategy
Dedicated vascular assessment
Mapping a patient’s lower limb arterial supply and venous drainage is a necessary prelude to treatment. The safest, least invasive, and most cost-effective way of achieving this is by dedicated vascular ultrasound. In good hands, this modality provides both structural and physiological information on arterial flow dynamics and directional venous competence that cannot be derived by CT angiography. Vascular ultrasound interpretation requires a specialised skill set, and the study results are very much dependent on the ultrasonographer’s ability. Geelong Vascular Ultrasound is our dedicated Vascular Laboratory for accurate, non-invasive vascular assessment, staffed by specialist Vascular Ultrasonographers. The clinic is open to outside referrals, which can be received by referral-net, or by fax to 03 5229 2819, and most patients with lower limb ulcers are offered mapping studies of their arteries and veins. Pensioners and health-card holders are bulk billed for all studies.
Arterial disease
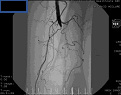
In most patients, arterial supply to the limbs can be improved by endovascular intervention, balloon angioplasty and intra-arterial stenting. Treatment is performed in-hospital under local anaesthetic with sedation, and few patients require longer than an overnight stay before resuming normal activity. Open surgical revascularisation by arterial endarterectomy or bypass grafting remains an option for consideration in some patients but has been largely replaced by the broad application of angio-intervention.
 |
 |
| Long length distal SFA occlusion recanalized and luminal calibre restored by intra-arterial stenting. |
Venous disease
A spectrum of venous disease underlies the presentation of chronic venous ulceration. Patients may have deep venous incompetence or obstruction, most often the consequence of previous DVT, and best managed with the appropriate application of graduated compression stockings. They may have superficial venous incompetence, the basis of varicose veins. They may have both. Superficial venous disease is best managed by endovenous ablative therapies, tolerated by young and old alike. The practice of open vein surgery in hospital, performed under general anaesthetic and usually including deep groin dissection, has been abandoned in most modern phlebology practices in the Western World.
It has been replaced with ambulatory outpatient treatment, endovenous laser ablation of incompetent main-stem veins, ultra-sound guided sclerotherapy, microphlebectomies, and visual microsclerotherapy. This is in line with the National Institute of Health and Care Excellence (NICE) guidelines, published in July 2013, which recommend ambulatory treatment of lower limb vein disease by laser or radiofrequency ablation ahead of any consideration for open surgery. Treatments at our Laser Vein Clinic are all performed under local anaesthetic, with ultrasound guidance. This provides patients with walk-in walk-out therapy, less perioperative discomfort, less invasive and inherently safer therapy, and an earlier return to normal activity.
Reducing venous hypertension by laser ablation of superficial vein incompetence provides for improved healing.
 |
| Reduction of venous hypertension by laser ablation of superficial vein incompetence provides for improved healing. |
Ulcer care
Most patients, on having their underlying arterial or venous disease addressed, return to the clinic of their General Practitioner for ulcer dressings until healing is complete. As a specialist wound care service, we are happy to provide advice on an appropriate dressing regimen, and to help organise community nurse home visits for regular dressings. Some patients will require more intensive surgical attention to manage their tissue loss. This is particularly the case in diabetics with foot ulcers for whom the combination of microangiopathy, autonomic neuropathy and peripheral sensory neuropathy often leads to the cascade of chronic ulceration, osteomyelitis and mechanical derangement of the foot. They are a particular challenge, requiring a multidisciplinary approach which we are keen to coordinate. Ulcer debridement, VAC dressings, split skin grafting, foot remodelling surgery, total contact casting, compression stocking supply and fitting, and stem cell therapy are all adjuncts we offer to help improve leg health and heal leg ulcers.
